The State of STIs — CDC Reports an Alarming Rise in Syphilis
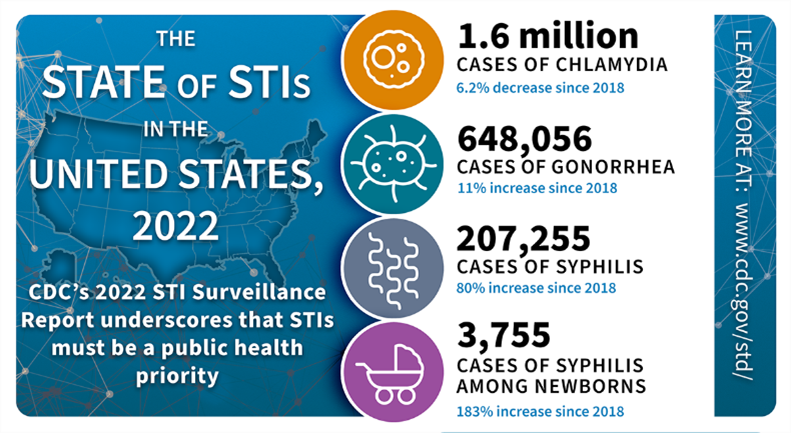
The Centers for Disease Control and Prevention released new surveillance data on sexually transmitted infections (STIs). There were 2.5 million cases of chlamydia, gonorrhea, and syphilis reported in the United States in 2022. Rates of gonorrhea and chlamydia remain high, and rates of syphilis have gone up an alarming 80% since 2018.
In 2022 there were:
- 1.6 million cases of chlamydia, which is a 6.2% decrease since 2018
- 648,056 cases of gonorrhea, which is an 11% increase since 2018
- 207,255 cases of syphilis, which is an 80% increase since 2018
- 3,755 congenital syphilis cases, which is an 183% increase since 2018
As always, the number of cases reported to the CDC is likely lower than the actual number of infections. Many STIs have no symptoms. A person could easily not know they were infected. Even STIs without symptoms, however, can lead to long-term health issues like infertility. This is why regular screening is so important.
“Today’s data show the magnitude of the STI epidemic in this country and highlight the importance of staying vigilant in our prevention, screening, and treatment efforts. The rise in syphilis—a disease we once came close to eradicating—is particularly alarming,” said ASHA’s President Lynn Barclay. “Treatment is prevention, but this only works with widespread screening efforts that reach everyone.”
While anyone who is sexually active can get an STI, the data show that some groups are more affected. This includes young people (ages 15 to 24), gay and bisexual men, pregnant people, and some racial and ethnic minority groups. It is important to understand that these disparities are not explained by behavior. Instead, they reflect other inequities in our society such as poverty and a lack of access to quality health care.
Laura Bachmann, MD, MPH, Acting Director, CDC’s Division of STD Prevention, stressed that we have to do a better job reaching all people: “There are no shortcuts, and we have to meet people where they are. Some people face tremendous barriers to STI prevention and health services. So, the most important work is often outside the clinic, whether it be reaching out to communities with testing, interviewing patients to offer services to their partners, or delivering treatment directly to someone.”
Keep reading for more data and infection-specific analysis:
- While chlamydia rates are up slightly in men, rates continue to be much higher in women (621.2 cases per 100,000 women compared to 363.7 cases per 100,000 men).
- 57.7% of all cases of chlamydia in 2022 were reported among young people ages 15 to 24.
It can be hard to identify trends in chlamydia infection because this STI usually has no symptoms. A decrease in chlamydia rates from year to year could mean that fewer people are getting the infection, or it could mean that fewer people are being screened. In 2020, for example, there were far fewer cases of chlamydia reported to the CDC. Most experts agree that this was because the pandemic prevented too many people from getting tested.
- Gonorrhea rates reached an historic low in 2009 but went on to increase every year through 2021. The 2022 data, shows a 9.2% decrease from the year before but the rates remain much higher than they were a decade ago.
- Since 2013, gonorrhea rates have been higher among men compared to women. This likely reflects cases in both men who have sex with men (MSM) and men who have sex with women only (MSW).
The bacteria that cause gonorrhea continues to evolve resistance to many of the antibiotics that were once used to treat it. It is estimated that half of gonorrhea infections in the U.S. in 2022 involved bacteria that were resistant to at least one antibiotic. The good news is that all of the strains in the U.S. still respond to ceftriaxone which is the recommended treatment. Still, public health experts are worried that the bacteria will continue to evolve and that we don’t have enough new antibiotics in development for when it does.
- The number of syphilis cases reported in 2022 was the highest since 1950. It represents a 17.3% increase from 2021 and a whopping 80% increase from 2018.
- Men who have sex with men (MSM) continue to be most impacted by syphilis, but rates of primary and secondary syphilis (the most contagious stages of the disease) among women have been increasing since 2013.
- In 2022, 3,755 cases of congenital syphilis were reported, including 282 congenital syphilis-related stillbirths and infant deaths.
The increase in syphilis among women has led to an alarming rise in congenital syphilis—babies born with the infection. The congenital syphilis rate was 102.5 cases per 100,000 live births in 2022. This represents a 30.6% increase from 2021. It is the highest reported rate in over 30 years. Congenital syphilis can lead to miscarriage, stillbirth, low birth weight, and other health issues (like blindness, deafness, or deformed bones). All pregnant people should be screened for syphilis.
- 49.8% of cases of chlamydia, gonorrhea, and syphilis in 2022 were among young people ages 15 to 24.
- 31.1% of all cases of chlamydia, gonorrhea, and primary and secondary syphilis were among non-Hispanic Black or African American people, even though they made up only 12.6% of the U.S. population.
One of the things that increases a person’s likelihood of getting an STI is their sexual network (a group of people that are connected through sexual behavior). Many factors—from the neighborhood in which someone lives to their access to health care—influence their sexual networks. These same factors also influence the STI rate within that sexual network. For example, chlamydia will likely spread more widely within a sexual network made up of people who do not readily have access to health care.