There Are Two New Drugs to Treat Gonorrhea
The FDA approved two new drugs to treat gonorrhea The new drugs—gepotidacin and zoliflodacin—are both new kinds of antibiotics and represent the first completely new treatment options in over thirty years.

About 1.6 million cases of chlamydia and 600,000 cases of gonorrhea are diagnosed in the United Sates each year. While some are diagnosed in clinics or through home tests, many people receive this diagnosis from their primary care clinician. A new study suggests that these patients may not be following through with treatment or getting the right antibiotics.
The study was conducted by researchers at Stanford University and the Centers for Disease Control and Prevention (CDC). Researchers looked at STI diagnoses in the PRIME registry which collects data from a representative sample of 2,000 primary care clinicians across the country. The goal was to see how quickly people diagnosed with one of these infections got treatment and if they received the treatment recommended by CDC guidelines. The results found a lot of gaps in how we treat these common STIs.
The researchers identified 6,678 cases of chlamydia and 2,206 cases of gonorrhea that had been diagnosed by a primary care clinician between 2018 and 2022. The majority of the cases—75% of chlamydia cases and 70% of gonorrhea cases—were treated within 30 days of the positive test results. That said, roughly 30% of chlamydia and gonorrhea cases were not treated at all.
This doesn’t mean the primary care clinician didn’t offer treatment. Instead, it usually means that the patient didn’t return for their results or got their results (possibly over the phone or through a portal) but didn’t return for the treatment.
STI testing and treatment in an office setting almost always requires two visits with a provider. This can be hard for people who lack health insurance, transportation, or a flexible work schedule. In addition, people who are unhoused, don’t have a permanent address, or don’t have a phone may never get their result.
The percentage of people who were treated varied among groups and communities. Women had a higher rate of treatment than men (78% vs 67% for chlamydia and 79% vs 51% for gonorrhea). Non-Hispanic White patients had the highest treatment rates of all racial/ethnic groups (76.8% for chlamydia and 73.5% for gonorrhea), and suburban residents had higher treatment rates (78% for chlamydia and 83% for gonorrhea) than those who lived in urban areas.
The time between diagnosis and treatment varied along similar lines. The median time was three days, but this was shorter for non-Hispanic Whites than other races, for women than men, and for suburban residents than urban residents.
Among the patients who did get treated, only 14% of those diagnosed with chlamydia and 39% of those diagnosed with gonorrhea were given the CDC’s recommended first-line antibiotics. The CDC recommends that people diagnosed with chlamydia take doxycycline while the recommended treatment for gonorrhea is a shot of ceftriaxone. Instead, most patients were given azithromycin.
The data doesn’t include why clinicians chose different treatments plans, but the researchers had some theories. Azithromycin can be given in a single oral dose which can be easier for patients than a 7-day course of doxycycline or a shot ceftriaxone. Still, this is concerning. There are reasons the CDC recommends certain treatment that include effectiveness and the growing risk of antibiotic resistance.
This study offers important insight into the gaps in treatment for chlamydia and gonorrhea. These infections are curable, but when left untreated they can cause long-term health issues including infertility. Moreover, timely treatment is an important part of prevention. People who don’t get tested and treated continue to pass the infection along to others.
The authors believe that patients and providers need additional education on the importance of timely treatment that follows recommendations.
Learn more about these two common—and curable—infections in this printable fact sheet. It covers the many things these two STIs have in common and includes information on testing, treatment, and staying healthy.
The FDA approved two new drugs to treat gonorrhea The new drugs—gepotidacin and zoliflodacin—are both new kinds of antibiotics and represent the first completely new treatment options in over thirty years.
A new report from the World Health Organization (WHO) warns of rising levels of drug-resistant gonorrhea. The data comes from reported cases of gonorrhea in 12 countries across five WHO regions.
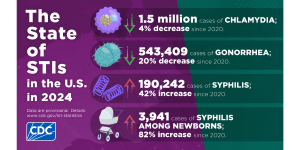
The CDC just released STI Surveillance Data for 2024 that show cases of chlamydia, gonorrhea, and syphilis are slowly declining.

On a recent episode of Love Island, a cast member sugested that we could blame our current STI epidemic on men who had sex with animals. She pointed to koalas with chlamydia as an example. There’s some truth here, but also a lot of misinformation.

There’s potential good news in gonorrhea prevention as a series of studies suggests that certain meningococcal B (MenB) vaccines can reduce the risk of gonorrhea.
Many people who take doxy PEP say it gives them peace of mind in their relationships and sex life. We sat down with Oscar Alexis, Efthimios, and Maxfield Haynes to talk about doxy PEP and get their perspective.

A clinical trial of a new antibiotic found that it works just as well as a current drug regimen for treating gonorrhea infections. This is important because the bacteria that causes gonorrhea has become resistant to most existing antibiotics.

The FDA just approved a new, fully at-home test for chlamydia, gonorrhea, and trichomoniasis. The tests, which is only for women, will be available without a prescription. Users can collect their own sample and have results in less than 30 minutes.
ASHA believes that all people have the right to the information and services that will help them to have optimum sexual health. We envision a time when stigma is no longer associated with sexual health and our nation is united in its belief that sexuality is a normal, healthy, and positive aspect of human life.
ABOUT
GET INVOLVED
ASHA WEBSITES
GET HELP
© 2025 American Sexual Health Association