When it comes to getting tested for sexually transmitted infections (STIs), there are some basic guidelines that apply to everyone who is sexually active regardless of sex, gender, or sexual partners. The most obvious piece of advice is to get tested right away if you have any symptoms like itching, burning, sores, or discharge. Of course, a lot of STIs have no symptoms, so it’s also a good idea to get tested when you have a new sexual partner or if you have multiple sexual partners.
There are other more specific screening recommendations for certain populations. For example, the CDC recommends that sexually active women under 25 get tested for chlamydia annually. There are also specific recommendations for gay, bisexual, and other men who have sex with men and for transgender and gender diverse persons. Missing from this list—heterosexual men. Instead, the CDC recommends “risk-based” screening for this population.
Why are there no universal screening recommendations for hetero men?
Screening recommendations are about setting priorities and making the biggest impact with the available resources. With limited funding, emphasis is on groups where infection is common and harm is greater. Young women, for example, are more susceptible to chlamydia infection, and the potential long-term consequences include infertility. Because infection is less common and the health impact less severe, widespread screening for STIs in hetero men is deemed “not cost effective.”
Should heterosexual men be a bigger priority in STI prevention efforts?
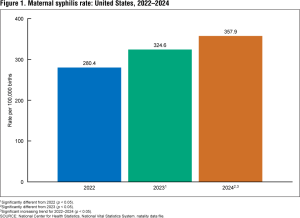
At the recent national STI Prevention Conference, Dr. Ina Park—author, sexual health MD, and UCSF professor—argued that we should be thinking differently about screening for hetero men. For one thing, heterosexual men are the ones passing STIs to heterosexual women. We can’t successfully address the rising rates of STIs—especially syphilis—in hetero women without getting men involved.
She also pointed to data that suggests risk-based screening of hetero men is not working in part because too few providers take a sexual health history. Without this information, they can’t accurately assess risk.
Dr. Park noted that men of color are disproportionately affected by STIs and could stand to gain the most if we are successful in STI control efforts among men. “Excluding hetero men from messaging around STI testing,” she concluded, “sends a message ‘your sexual health is not a priority.’”
Ahead of her presentation, Dr. Park took her case to social media with her characteristic humor and a survey.