There Are Two New Drugs to Treat Gonorrhea
The FDA approved two new drugs to treat gonorrhea The new drugs—gepotidacin and zoliflodacin—are both new kinds of antibiotics and represent the first completely new treatment options in over thirty years.
A new report from the World Health Organization (WHO) warns of rising levels of drug-resistant gonorrhea. The data comes from reported cases of gonorrhea in 12 countries across five WHO regions.
Gonorrhea is one of the most common bacterial sexually transmitted infections (STIs) in the world with an estimated 82 million cases across the globe each year. In the United States, the Centers for Disease Control and Prevention (CDC) estimate 1.6 million cases of gonorrhea each year.
Many people who get gonorrhea won’t have any symptoms. Those who do may experience discharge from the penis or vagina and a burning sensation when they pee. Gonorrhea can also cause swollen testicles. If left untreated, gonorrhea can cause further health issues including infertility in both men and women.
Gonorrhea is caused by the bacterium, Neisseria gonorrhoeae, that continues to evolve to avoid antibiotics. This is referred to as developing antibiotic resistance. Over the last eighty years, gonorrhea has developed resistance to sulfanilamides, penicillins, tetracyclines, and fluoroquinolones. That leaves just one class of antibiotics—cephalosporins—as the only effective treatment we have left.
In the U.S. people with uncomplicated gonorrhea are given a single dose shot of ceftriaxone (which is a cephalosporin). Some are also given a dose of oral azithromycin. There have been cases in a number of countries in which this treatment alone was not enough. Those patients have all been cured of gonorrhea but have had to take a combination of antibiotics. The fear is that cases like these will begin to happen more often as gonorrhea becomes increasingly resistant to drugs we use to fight it.
The data from WHO’s Enhanced Gonococcal Antimicrobial Surveillance Program (ESGAP) report show that resistance to all available drugs rose in recent years. In 2022, only 0.8% of the Neisseria gonorrhoeae samples collected were resistant to ceftriaxone, by 2024 it was 5% of samples. Similarly, resistance to cefixime (another first-line cephalosporin) rose from 1.7% to 11% and resistance to azithromycin rose from 0.5% to 4%. Even more alarming, 95% of Neisseria gonorrhoeae isolates were found to be resistant to ciprofloxacin (often referred to as cipro).
There is good news, however, two new antibiotics— zoliflodacin and gepotidacin—were successful in clinical trials and may be available soon.
Of course, prevention and screening continue to be important. Gonorrhea is considered a “discharge disease” because it is spread through infected bodily fluids such as semen and cervical secretions. Condoms have been proven to provide excellent protection against discharge diseases.
Doxy PEP—the practice of taking doxycycline after sex to prevent bacterial STIs—can also provide some protection against gonorrhea. Doxy PEP is not as effective as it is against chlamydia and syphilis, likely because of the resistance the bacterium has developed, but it can reduce the risk of gonorrhea by 50%.
Screening and treatment are also an important part of preventing the spread of gonorrhea as well as the long-term health issues it can cause if left untreated. The Centers for Disease Control and Prevention (CDC) recommend yearly gonorrhea screening for:
MSM who have multiple partners, anonymous partners, or partners who have an STI may want to be screened more often. Screening should be done at all possible sites of infection including the penis, throat, and anus.
Tracking antibiotic resistance in gonorrhea is also very important, but some areas lack the resources to do it. WHO officials called on countries around the world to invest in increased and improved surveillance so that we have the data we need to stay ahead of antibiotic resistance.
The FDA approved two new drugs to treat gonorrhea The new drugs—gepotidacin and zoliflodacin—are both new kinds of antibiotics and represent the first completely new treatment options in over thirty years.
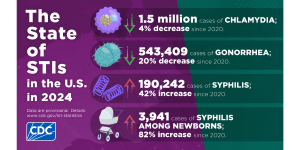
The CDC just released STI Surveillance Data for 2024 that show cases of chlamydia, gonorrhea, and syphilis are slowly declining.

On a recent episode of Love Island, a cast member sugested that we could blame our current STI epidemic on men who had sex with animals. She pointed to koalas with chlamydia as an example. There’s some truth here, but also a lot of misinformation.

There’s potential good news in gonorrhea prevention as a series of studies suggests that certain meningococcal B (MenB) vaccines can reduce the risk of gonorrhea.
Many people who take doxy PEP say it gives them peace of mind in their relationships and sex life. We sat down with Oscar Alexis, Efthimios, and Maxfield Haynes to talk about doxy PEP and get their perspective.

About 1.6 million cases of chlamydia and 600,000 cases of gonorrhea are diagnosed in the United Sates each year. A new study suggests that these patients may not be following through with STI treatment or getting the right antibiotics.

A clinical trial of a new antibiotic found that it works just as well as a current drug regimen for treating gonorrhea infections. This is important because the bacteria that causes gonorrhea has become resistant to most existing antibiotics.

The FDA just approved a new, fully at-home test for chlamydia, gonorrhea, and trichomoniasis. The tests, which is only for women, will be available without a prescription. Users can collect their own sample and have results in less than 30 minutes.
ASHA believes that all people have the right to the information and services that will help them to have optimum sexual health. We envision a time when stigma is no longer associated with sexual health and our nation is united in its belief that sexuality is a normal, healthy, and positive aspect of human life.
ABOUT
GET INVOLVED
ASHA WEBSITES
GET HELP
© 2025 American Sexual Health Association