
FDA Approves New Version of PrEP—Just Two Shots A Year
The FDA has approved lenacapavir as a form of pre-exposure prophylaxis (PrEP), offering a new option for HIV prevention requiring only two shots per year.
Doxy PEP—or doxycycline post-exposure prophylaxis—is a sexual health strategy that involves taking an oral antibiotic after condomless sex to prevent chlamydia, gonorrhea, and syphilis.
This strategy comes at a time when bacterial STIs are on the rise. Recently released data from the CDC showed there were 2.5 million cases of chlamydia, gonorrhea, and syphilis reported in the United States in 2022. Cases of chlamydia and gonorrhea—the two most common reportable STIs—have remained high for many years, and syphilis cases have skyrocketed recently. The number of primary and secondary syphilis infections in 2022 was 80% higher than in 2018.
Doxy PEP is the first new prevention method for bacterial STIs, and many experts believe it will be an important tool in our fight against this epidemic.
Doxy PEP is the strategy of taking the antibiotic doxycycline after condomless oral or anal sex to prevent chlamydia, gonorrhea, or syphilis.
Doxy PEP is intended for adult men who have sex with men and transgender women who have sex with men especially those who have had an STI in the last year. Health care providers may also suggest it to people in this community who have more than one partner.
Some providers might offer doxy PEP to cisgender men who have sex with women if they’ve had condomless sex with more than one partner, especially if they’ve had a bacterial STI like syphilis in the past year. Research with this group is still ongoing.
So far, research has not found doxy PEP to be effective in preventing STIs in cisgender women who have penis-in-vagina sex. More research is being done on this and other populations like adolescents.
You need a prescription for doxy PEP. You can talk to your health care provider or go to a sexual health clinic like those that offer STI testing. Because you have to take doxy PEP quickly after having condomless sex, it’s a good idea to talk to your health care provider about this before you need it.
People using doxy PEP take 200 mg of doxycycline (usually two 100 mg pills) within 72 hours of condomless sex though sooner is better. Doxy PEP can be used every time you have condomless sex, but you shouldn’t take more than 200 mg of doxycycline in a 24-hour period.
Doxycycline is typically inexpensive and usually covered by insurance. Some places may give out doxy PEP for free.
Doxycycline is a common antibiotic that many of us have taken for other infections. Like other antibiotics, it may upset your stomach. Take it with lots of water and try not to lie down for half an hour. Doxycycline may also make you more sensitive to the sun so you should try to avoid prolonged exposure while taking it.
Some people may have more serious reactions. Talk to a health care provider if you have other symptoms—like a bad headache or blurred vision—after taking it.
We have been told over the years that overuse of antibiotics is a problem because it can lead to antibiotic-resistant bacteria (infections that don’t respond to the drugs we have to treat them). The research that has been done so far has not found that doxy PEP increases drug resistance in patients, but scientists will have to keep monitoring it.
Gonorrhea is one of the bacteria that has become resistant to some antibiotics. In fact, about 25% of strains of gonorrhea are resistant to doxycycline. This may be why doxy PEP doesn’t work as well against gonorrhea as it does against chlamydia and syphilis.
Doxy PEP only protects against bacterial STIs. It does not protect against viruses like MPox, HIV, or herpes. The best protection against MPox is the vaccine. If you think you are at risk for HIV, talk to your health care provider about Post-Exposure Prophylaxis (PEP) and Pre-Exposure Prophylaxis (PREP).
Yes. It’s important to keep up with STI screenings and to get checked if you have any symptoms. The CDC recommends that MSM be tested for chlamydia, gonorrhea, and syphilis at least annually and more often (every 3 to 6 months) if you are at increased risk because of HIV infection or multiple partners. Talk to your health care provider about how often you should be screened.
On this episode of the Sex+Health podcast we talk with Jaylan Daniels, who tells us all about doxy PEP and why he chose to include it as part of his health care regimen.
Download our printable fact sheet on doxy PEP, covering who can benefit from taking doxy PEP, how its used, side effects, concerns about antibiotic resistance, and STI testing.

The FDA has approved lenacapavir as a form of pre-exposure prophylaxis (PrEP), offering a new option for HIV prevention requiring only two shots per year.

On a recent episode of Love Island, a cast member sugested that we could blame our current STI epidemic on men who had sex with animals. She pointed to koalas with chlamydia as an example. There’s some truth here, but also a lot of misinformation.

A new report from the Centers for Disease Control (CDC) shows that we’re missing opportunities to prevent congenital syphilis and save lives.
Currently, condoms are the only widely available, proven method for reducing transmission of HIV and other sexually transmitted infections (STIs) during sex. Condoms work.

Anal sex may have once been thought of more taboo than other sexual behaviors, but today we know it’s a perfectly normal way to find sexual pleasure.
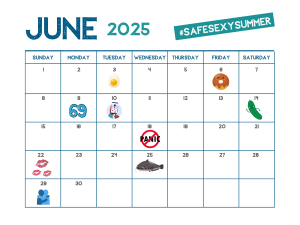
It’s time to celebrate the start of summer! June is filled with national observances to help you start the summer off right. We’re here to help make June the start of a #safesexysummer.

There’s potential good news in gonorrhea prevention as a series of studies suggests that certain meningococcal B (MenB) vaccines can reduce the risk of gonorrhea.

There is new guidance on pain management for IUD insertion and acknowledgement that providers often underestimate the pain patients feel during their procedures.
ASHA believes that all people have the right to the information and services that will help them to have optimum sexual health. We envision a time when stigma is no longer associated with sexual health and our nation is united in its belief that sexuality is a normal, healthy, and positive aspect of human life.
ABOUT
GET INVOLVED
ASHA WEBSITES
GET HELP
© 2025 American Sexual Health Association