When you think of HIV prevention, condoms are probably the first thing that comes to mind (which is great, because they should! Condoms are a proven method to reduce your risk for HIV and other sexually transmitted infections during intercourse.) But there is another option for those who may be at higher risk for HIV—PrEP.
PrEP stands for pre-exposure prophylaxis. The word prophylaxis means to prevent or control the spread of an infection or disease. The goal of PrEP is to prevent HIV infection from taking hold if you are exposed to the virus.
PrEP involves taking medication to prevent HIV infection. Oral PrEP involves taking a pill once daily to prevent HIV infection in someone who is HIV-negative. Currently there are two pills approved for PrEP:
- Truvada (for anyone at-risk for HIV) and
- Descovy (for those at risk except for people assigned female gender at birth who may be at risk for HIV from vaginal sex).
When taken consistently, every day, oral PrEP has been shown to reduce the risk of HIV infection in people who are at high risk by about 99%.
The newest PrEP option—Apretude—is given as an injection every two months (following two initiation doses given a month apart). This option is approved to reduce the risk of sexually acquired HIV in at-risk adults and adolescents weighing at least 77 pounds.
Who should take PrEP?
So who is PrEP recommended for? The Centers for Disease Control and Prevention (CDC) offers these guidelines on people who should consider taking PrEP:
You have had anal or vaginal sex in the past 6 months and you:
- have a sexual partner with HIV (especially if the partner has an unknown or detectable viral load),
- have not consistently used a condom, or
- have been diagnosed with a sexually transmitted infection in the past 6 months.
You inject drugs and you:
- have an injection partner with HIV, or
- share needles, syringes, or other drug injection equipment (for example, cookers).
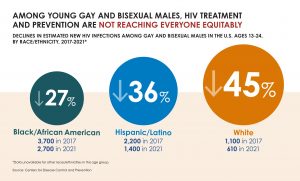
While PrEP is recommended for different groups, it has received the most attention in the gay community. Gay and bisexual men are disproportionately affected by HIV. PrEP has been endorsed as an important prevention tool by a number of prominent activists and organizations, including the Human Rights Campaign, the Gay Men’s Health Crisis, AIDS United, and the World Health Organization.
PrEP + Condoms
PrEP shouldn’t be considered a replacement for condoms. Rather, PrEP offers a new, highly effective prevention option—another tool in the HIV prevention toolbox that fits alongside condoms, not as a replacement. After all, while PrEP helps prevent HIV infection, condoms offer protection against a host of other STIs as well.
Despite the promise offered by PrEP, it isn’t necessarily the right choice for everyone. In addition to requiring taking pills or getting an injection consistently, those on PrEP are also advised to see health care provider regularly for follow up and get tested for HIV every three months. But for those willing to take on the commitment, PrEP offers the promise of a highly effective way to prevent HIV.
Where to Find PrEP
If you are interested in PrEP, you’ll want to find a provider who is both knowledgable about PrEP and supportive of your decision. If you have a regular health care provider, you can start there. The PrEP locator below can also help you find a provider in your area.
Most insurance plans and state Medicaid programs cover PrEP. Under the Affordable Care Act, PrEP must be free under almost all health insurance plans.
The Ready, Set, PrEP program provides access to PrEP medications for free to people who qualify. You can apply for the Ready, Set, PrEP program if you:
- Don’t have health insurance coverage for prescription drugs
- Have taken an HIV test and received a negative result before starting the program
- Have a prescription for PrEP
- Live in the United States including tribal lands and territories