
Living with HIV/AIDS
Life continues after becoming HIV positive. Thanks to new treatments, many people with HIV are living long, healthy lives.
HIV:
Fast Facts
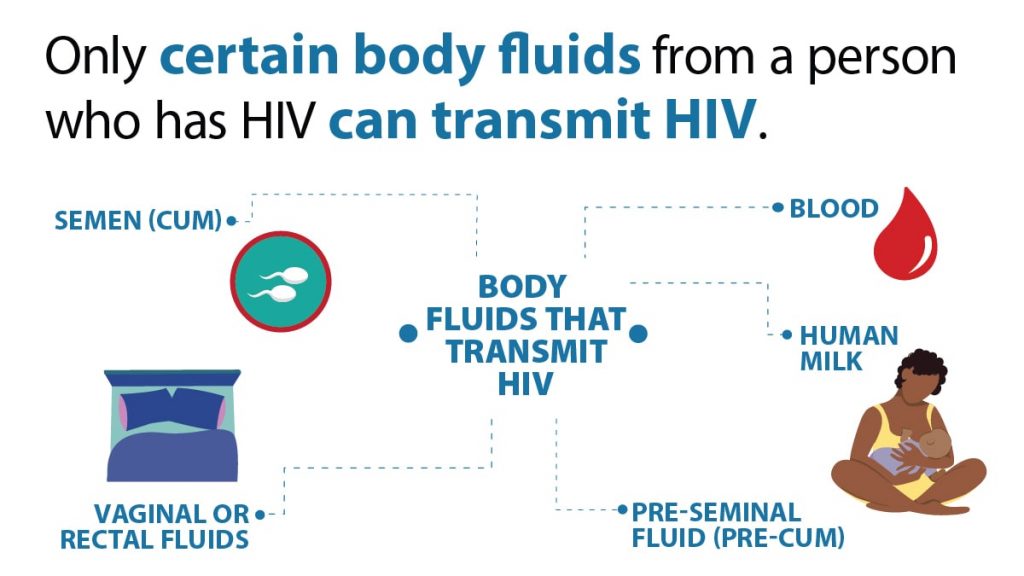
HIV can be transmitted through the blood, sexual fluids (semen, preseminal fluid, rectal fluid, or vaginal fluid) or breast milk of an HIV-infected person. People can get HIV one of these fluids enters the body by way of the mucous membranes (the soft, moist skin found in any opening of the body) or the bloodstream.
The virus can be passed during vaginal, anal or oral sex with a HIV-infected person. An HIV-infected mother can transmit HIV to her infant during pregnancy, delivery or while breastfeeding. People can also become infected with HIV when using injection drugs through sharing needles and other equipment (or works) including cookers and cottons with someone who is infected.
The risk of transmission varies with the type of exposure (e.g. sexual, needle sharing, etc.) The Centers for Disease Control and Prevention (CDC) offers a table quantifying the this HIV transmission risk that comes from different types of exposures.
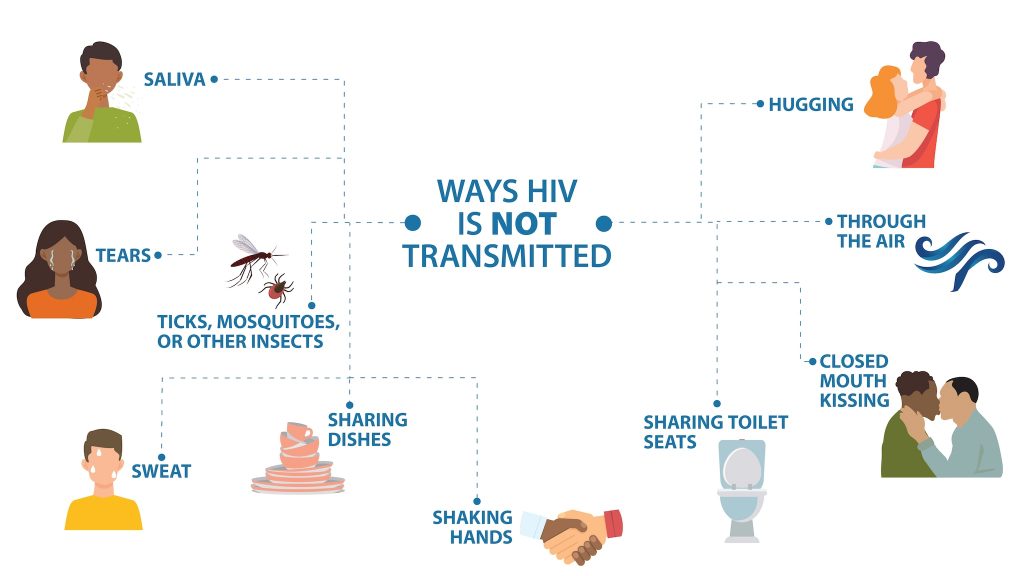
No. HIV is not transmitted by day-to-day contact in social settings, schools or in the workplace. You cannot be infected by shaking someone’s hand, by hugging someone, by using the same toilet or drinking from the same glass as an HIV-positive person, playing sports with or by being exposed to coughing or sneezing by anyone living with HIV. There is no evidence that HIV is spread through kissing. So you should not be fearful of interacting with persons who are living with the disease.
Many people infected with HIV don’t know that they have become infected, because they don’t have any symptoms of infection. But some people do experience a flu-like illness with fever, rash, joint pains and enlarged lymph nodes. If an immune reaction to HIV occurs, it usually takes place between 2 to 4 weeks after HIV infection has happened.
A person with HIV may look healthy and feel good, but they can still pass the virus to others, especially during the initial infection period. You cannot tell if someone has HIV by just looking at them. The only way to determine whether HIV is present in a person’s body is by testing.
AIDS (acquired immune deficiency syndrome) is a disease caused by HIV. HIV infects cells of the human immune system and destroys or impairs their function. Infection with this virus leads to slow destruction of a persons’ immune system making them more susceptible to many kinds of infections. Once a person with HIV develops any one of a number of rare infections or cancers—tuberculosis, pneumonia, candidiases or tumors—they are said to have AIDS.
The introduction of powerful anti-retroviral therapies has made a dramatic impact. With antiretroviral therapy (called ART), people with HIV can live long and healthy lives. The goal of HIV treatment is to reduce the amount of virus in the blood, called viral load. Treatment can reduce the viral load to undetectable levels, and the virus cannot be passed on to HIV-negative partners through sex. This called U=U: undetectable. equals untransmitable.
The U.S. blood supply is very safe. The risk for HIV from blood products and donated organs or tissues is extremely low because of rigorous testing. There is also no risk for HIV when donating blood.
Yes. Sharing needles puts injecting drug users (IDUs) at risk for many blood-borne diseases, including hepatitis B and C, as well as HIV. It is recommended that a person never reuse or share works (cookers, cottons, syringes, needles, water.) New needles, from a reliable source, should be used every time. Swabbing the sight with alcohol can help prevent other types of infections. Safely dispose of needles after using.
If new equipment is not available, syringes disinfected to reduce the risk of transmission. This fact sheet from CDC discusses the process.
There are lots of ways to prevent HIV.

Life continues after becoming HIV positive. Thanks to new treatments, many people with HIV are living long, healthy lives.
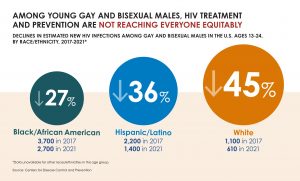
While CDC reported a decline in overall new HIV infections, disparities in HIV prevention and treatment remain.

A joint investigation by the CDC and the New Mexico Health Department has confirmed that an unlicensed medi-spa is responsible for at least three cases of HIV.

Anytime is the right time to promote HIV prevention and advocacy and there are specific observations recognized throughout the year when it’s especially good to be involved.

HIV and Pregnancy There is a lot to think about when you want to have a baby or when a baby is on the way. One important step is to learn about HIV. There are good reasons to get an HIV test if you are
PrEP stands for pre-exposure prophylaxis. The word prophylaxis means to prevent or control the spread of an infection or disease. The goal of PrEP is to prevent HIV infection from taking hold if you are exposed to the virus.

A new study found that opt-out screenings for all patients in emergency departments caught numerous cases of syphilis and HIV that would have gone undetected under other screening protocols.

The only way to tell you have HIV is get tested. Testing is recommended at least once for everyone, and may be recommended more often for some. Testing can be quick, easy and confidential.
ASHA believes that all people have the right to the information and services that will help them to have optimum sexual health. We envision a time when stigma is no longer associated with sexual health and our nation is united in its belief that sexuality is a normal, healthy, and positive aspect of human life.
ABOUT
GET INVOLVED
ASHA WEBSITES
GET HELP
© 2025 American Sexual Health Association