There’s potential good news in gonorrhea prevention. A series of studies suggests that certain meningococcal B (MenB) vaccines can reduce the risk of gonorrhea. As a result, public health experts in England have decided to offer the vaccine to people more likely to be exposed to gonorrhea.
In the United States, gonorrhea is the second most common reported bacterial STI. There were over 600,000 cases of gonorrhea diagnosed in this country in 2023. Because so many cases of gonorrhea have no symptoms, many people never get tested. That means it is likely there are far more annual cases. In fact, the CDC estimates there are actually 1.6 million case each year.
Preventing Gonorrhea
We’ve been able to cure gonorrhea for nearly 100 years, but we are running out of medications that work. The bacterium that causes gonorrhea has been steadily changing to evade entire classes of antibiotics. As early as the 1940s, these bacteria were resistant to sulfanilamides. By the 1980s they were resistant to penicillins and tetetracyclines. In 2007, the CDC stopped recommending fluoroquinolones. This leaves cephalosporins as the only effective treatment. This makes prevention even more important.
We already have some effective prevention tools. Condoms block the exchange of semen and cervical secretions which is how the bacteria are spread. Doxy PEP involves taking an oral antibiotic after condomless sex to prevent STIs. It has been found to be about 50% effective against gonorrhea and 80% effective against chlamydia and syphilis.
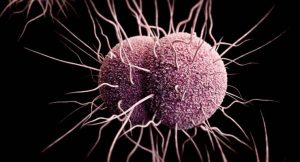
There is no vaccine against gonorrhea, which is caused by the bacterium Neisseria gonorrhoeae. But there is a vaccine against meningococcal meningitis, caused by the bacterium Neisseria meningitidis. These bacteria are genetically similar. Scientists have been studying whether meningococcal B (MenB) vaccines provide any protection against gonorrhea. Two new reviews of research suggest they do.
New Research on an Existing Vaccine
These reviews—conducted by researchers in Hungary and Greece—found that the incidence of gonorrhea was lower in people who received the 4CMenB vaccine than it was in individuals who weren’t vaccinated or had received other meningococcal vaccines.
One of the components in the vaccine is called OMV or outer membrane vesicles. OMV are naturally released the type of bacteria that cause meningococcal meningitis and gonorrhea. OMV mimic the outside of bacteria and resemble a pathogen but they are non-living so they can’t cause disease. This makes them an effective vaccine delivery system.
The Hungarian researchers analyzed seven studies, six of which studied the 4CMenB vaccine. They found a pooled vaccine effectiveness (VE) of 38% against gonorrhea infection. The pooled VE went up slightly—to 41%—when they looked only at the studies of the 4CMenB vaccine.
Similarly, the researchers in Greece analyzed nine studies, eight of which studied the 4CMenB vaccine. They found a pooled VE of 30% against gonorrhea. They concluded, “While randomized clinical trials are necessary, the findings of this systematic review and meta-analysis highlight the potential effectiveness of OMV-based vaccines in terms of gonorrhea prevention.”