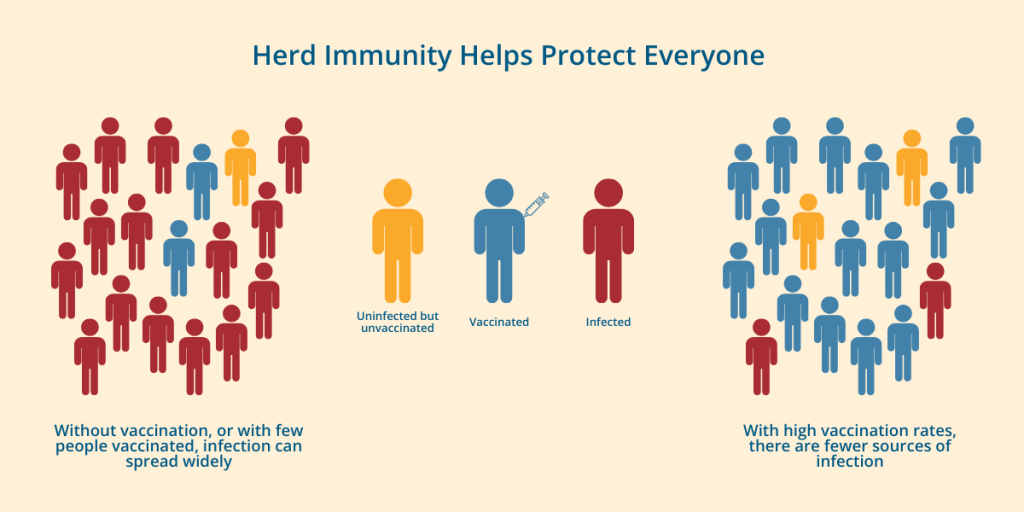
We’ve known for years that the HPV vaccine protects people who have received it from the high-risk types of the virus that are most likely to cause cancer. Now new research shows that widespread vaccination even protects those who haven’t gotten the shot. This study proves that it is possible to reach herd immunity for HPV.
Human papillomavirus (HPV) is a highly contagious virus that is spread through skin-to-skin contact. There are over 100 different types of HPV. Some types can cause genital warts while other types can cause cancer, including cancer of the cervix, vulva, vagina, penis or anus, as well as cancer in the back of the throat. These are referred to as “high-risk types.”
The HPV vaccine was introduced in 2006. The first two formulations of the vaccine—the 2-valent and 4-valent versions—protected against two or four of the high-risk types of HPV. The current vaccine, which was introduced in 2014, protects against nine types of HPV. It is referred to as the 9-valent vaccine.
The HPV vaccine is part of recommended vaccinations given to adolescents at age 11-12. It can be given as early as age 9 and is now approved for people into their 40s. Though it was originally only for young women, the vaccine is now recommended for everyone regardless of biological sex or gender.
Study Shows How HPV Vaccine Offers Protection
Researchers at Albert Einstein College of Medicine in New York wanted to determine how well the vaccine was working over time. They conducted six studies with young people in Cincinnati between 2006 and 2023. Participants ranged in age from 13 to 26 at the time of enrollment. The initial study was done just before the HPV vaccine became available.
Over the 17-year study period, HPV vaccination rates rose from 0% to 82%. The researchers found that as vaccination coverage increased, the rates of HPV infection dropped dramatically among vaccinated participants:
- Infections from HPV types covered by the 2-valent vaccine fell by 98.4%
- Infections from types covered by the 4-valent vaccine dropped by 94.2%
- Infections from types covered by the 9-valent vaccine declined by 75.7%
According to the authors, these results are proof that the vaccines are working among those young people who received them. Aislinn DeSieghardt, clinical research coordinator at Cincinnati Children’s Hospital Medical Center and one of the authors, said, “Our analysis of the data indicates that those reductions in infection rates were primarily due to the vaccine’s introduction and not because of changes in sexual behavior or other factors.”
But the researchers went beyond that and looked at rates of high-risk types of HPV among unvaccinated people in the same age groups. Among unvaccinated women:
- Infections with HPV types covered by the 2-valent vaccine decreased by 71.6%
- Infections with HPV types covered by the 4-valent vaccine dropped by 75.8%
Dr. Jessica Kahn, a professor of Pediatrics at Einstein, was the lead author on this study. She explained that they found “… clear evidence of herd immunity, meaning when enough people are vaccinated, the vaccine indirectly protects unvaccinated people by reducing overall virus transmission.” Dr. Kahn also explained that there was not enough data to confirm herd immunity with the 9-valent shot because it is newer, but the outcome looks promising.
Unfortunately, vaccination rates in the U.S. have stalled as anti-vax rhetoric has heated up. HPV vaccination rates increased every year from 2013 to 2021. However, only 62.9% of teens were “up to date” on their HPV vaccination in 2024, a rate that was about the same as the prior two years. Public health experts worry that this could signal the start of trend away from HPV vaccines.
The results of the current study show that widespread vaccination can prevent HPV and HPV-related cancers. But this can only work if we keep vaccination rates high.