Screening More Often
The official recommendations have not yet been finalized, but it is likely that people who use HPV self-collection and test negative will be told to come back in three years. People who have their provider take a sample and test negative for HPV don’t need to come back for five years. (People who get only pap tests are also told to get tested every three years.)
Follow Up
Anyone who tests positive for HPV will have to see their provider for additional tests.
If you test positive for HPV types 16 or 18, your provider will probably ask you to come in for colposcopy (see below). This is the same follow up they would do if a Pap test came back abnormal.
If you did self-collection and test positive for another, lower-risk type of the virus, your provider might have you return to the office for a Pap test. This is one outcome where the procedure is different for self-collection. When a provider collects samples for an HPV test, the same sample can be used for cytology, and you’d only have to re-test if that test comes back abnormal.
Most HPV tests come back negative and no follow-up is required.
Colposcopy/Biopsy
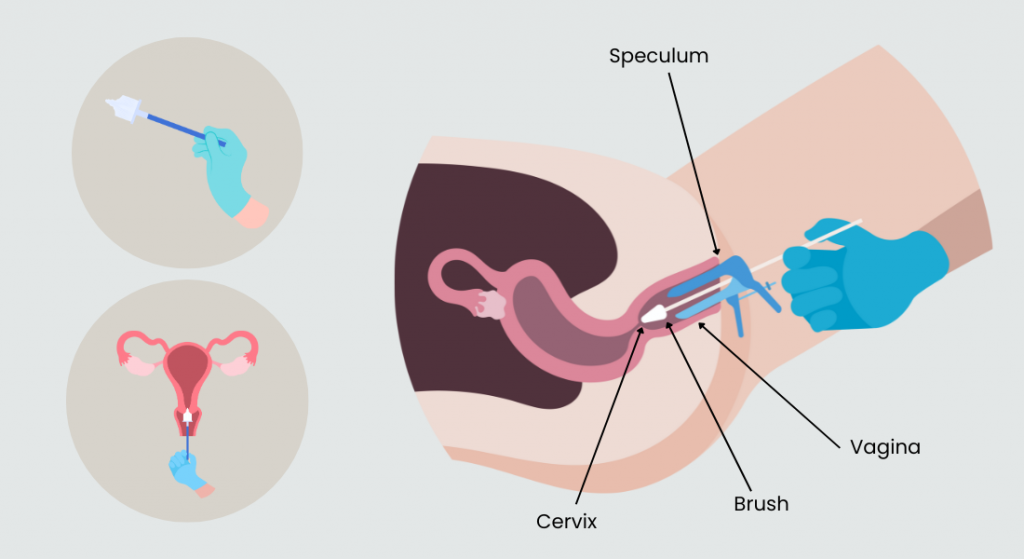
If your HPV test comes back positive for types 16 or 18 or your Pap test comes back abnormal, your provider will likely ask you to come back for colposcopy. This is a procedure that looks closely at the cervix with a special lighted microscope (called a colposcope). It is done in a provider’s office during a speculum exam. It does not hurt but may be uncomfortable.
If your provider sees something that looks like it might be cancerous or precancerous, they may cut out a small piece of tissue from the cervix that can be examined more closely in a lab. This is called a biopsy.
Biopsies can pinch or hurt for a few minutes and may cause cramping similar to menstrual cramps. Talk to your provider about what to expect, and what you can do for pain before or after the procedure.
A Great New Option
HPV Self-Collection is a great new option for cervical cancer screening. It is easy to do, and lets you avoid a speculum exam which many people find uncomfortable.
Self-collection was only recently approved, but the hope is that it becomes available not just in gynecologists’ offices and women’s health clinics, but in other convenient places like primary care offices, urgent cares, ERs, mammogram facilities, mobile health clinics, and even pharmacies.
The easier we make it for everyone to get screened for cervical cancer, the faster we can meet our goal of eliminating this disease in the United States.