Learn About Condoms
Currently, condoms are the only widely available, proven method for preventing pregnancy and reducing transmission of HIV and other sexually transmitted infections (STIs) during sex. Condoms work.

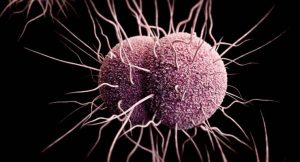
A new study suggests emergency departments should be providing universal screening for syphilis and HIV. The results, presented at the Conference on Retroviruses and Opportunistic Infections, found that opt-out screenings for all patients caught numerous cases of both infections that would have gone undetected under other screening protocols.
The paper was presented by Dr. Kimberly Stanford of the University of Chicago Medical Center. In 2019, the hospital implemented an opt-out universal screening system for both syphilis and HIV. All patients under 65 who had not been screened in the previous year were tested for both infections unless they declined. An alert would pop up on the patient’s electronic medical record during triage so the provider doing intake could mention the testing practice and offer a chance for the patient to opt-out. If not addressed at that time, the alert would pop up any time a provider opened the record.
More than 37,000 patients were screened during the first two years of this program. In that time, there were 624 patients positive for syphilis tests, 83 new HIV diagnoses, and 21 acute cases of HIV.
Stanford and her team analyzed the records to see how many of these cases would have been caught under other screening systems that based on orders or population. Who gets tested under an orders-based screening system depends on the issues they present with and the other tests they are being given. Who gets tested under a population-based screening system depends on characteristics of each patient such as their age, their pregnancy status, and their behavior.
These systems can be easier to implement and less taxing on hospital resources including staff and laboratory expenses. This new research, however, shows that such systems can miss many cases of both syphilis and HIV.
Syphilis is curable if caught early but can cause long-term health consequences when not treated. Syphilis can be especially dangerous during pregnancy. Congenital syphilis can cause miscarriage, stillbirths, prematurity, and low birth weight. Babies born with syphilis can have deformed bones, severe anemia, blindness, deafness, or other neurological issues.
Similarly, while there is no cure for HIV, early diagnoses and treatment can ensure a person stays healthy longer and is key to preventing transmission to others. It is also the key to preventing transmission during pregnancy.
Opt-out strategies cast a wider net and are able to catch STIs that might otherwise have gone undetected. They can also help eliminate provide bias about who should get tested as well as the stigma people may feel when a provider suggests STI testing. People often feel less judged if a provider says something like, “It is our policy to test everyone for syphilis unless they refuse.” The CDC has highlighted opt-out strategies as an effective way to increase the number of young people screened for other STIs including chlamydia and gonorrhea. The CDC also recommends opt-out testing for HIV.
This study shows that switching to such a system in an emergency department is feasible and can improve screening rates specifically for syphilis and HIV. ED visits are an important interaction with the healthcare system especially for people who might not otherwise see providers. As this study tells use, they are often a missed opportunities to expand STI testing. Switching to a universal opt-out system could change that.
Currently, condoms are the only widely available, proven method for preventing pregnancy and reducing transmission of HIV and other sexually transmitted infections (STIs) during sex. Condoms work.

At the end of 2025, the American Cancer Society released its new cervical cancer screening guidelines. In January 2026, the Health Resources and Services Administration endorsed a new set of guidelines as well. Both suggest HPV screening with self collected samples is an acceptable option.

Research suggests that only one dose of the HPV vaccine may be effective enough to prevent HPV-related disease, including cancer.

Australia has been a leader in HPV-prevention and cervical cancer screening for decades. Because of this, it is now close to eliminating cervical cancer entirely. However, recent drops in vaccination and screening rates threaten this progress.
The FDA approved two new drugs to treat gonorrhea The new drugs—gepotidacin and zoliflodacin—are both new kinds of antibiotics and represent the first completely new treatment options in over thirty years.

The American Cancer Society (ACS) released new recommendations for cervical cancer screening that focus on HPV testing and approve the use of self-collected samples. The recommendations also clarify the age at which screening should start and stop.
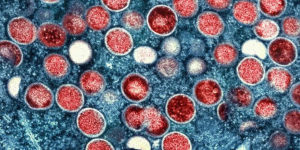
Public health officials in England announced that they have identified a new combined type of mpox. Tests show the virus was a unique mix of the two known types of mpox and experts are concerned about what this means for future spread of the virus.

A committee that advises the Centers for Disease Control and Prevention (CDC) made an alarming change to the recommendations for the hepatitis B vaccine that will leave some infants unprotected.
ASHA believes that all people have the right to the information and services that will help them to have optimum sexual health. We envision a time when stigma is no longer associated with sexual health and our nation is united in its belief that sexuality is a normal, healthy, and positive aspect of human life.
ABOUT
GET INVOLVED
ASHA WEBSITES
GET HELP
© 2026 American Sexual Health Association