
The HPV Vaccine Prevents Cancer
In the U.S., HPV infections are estimated to cause about 37,300 cases of cancer. The HPV vaccine can prevent over 90% of these cancers from ever developing.

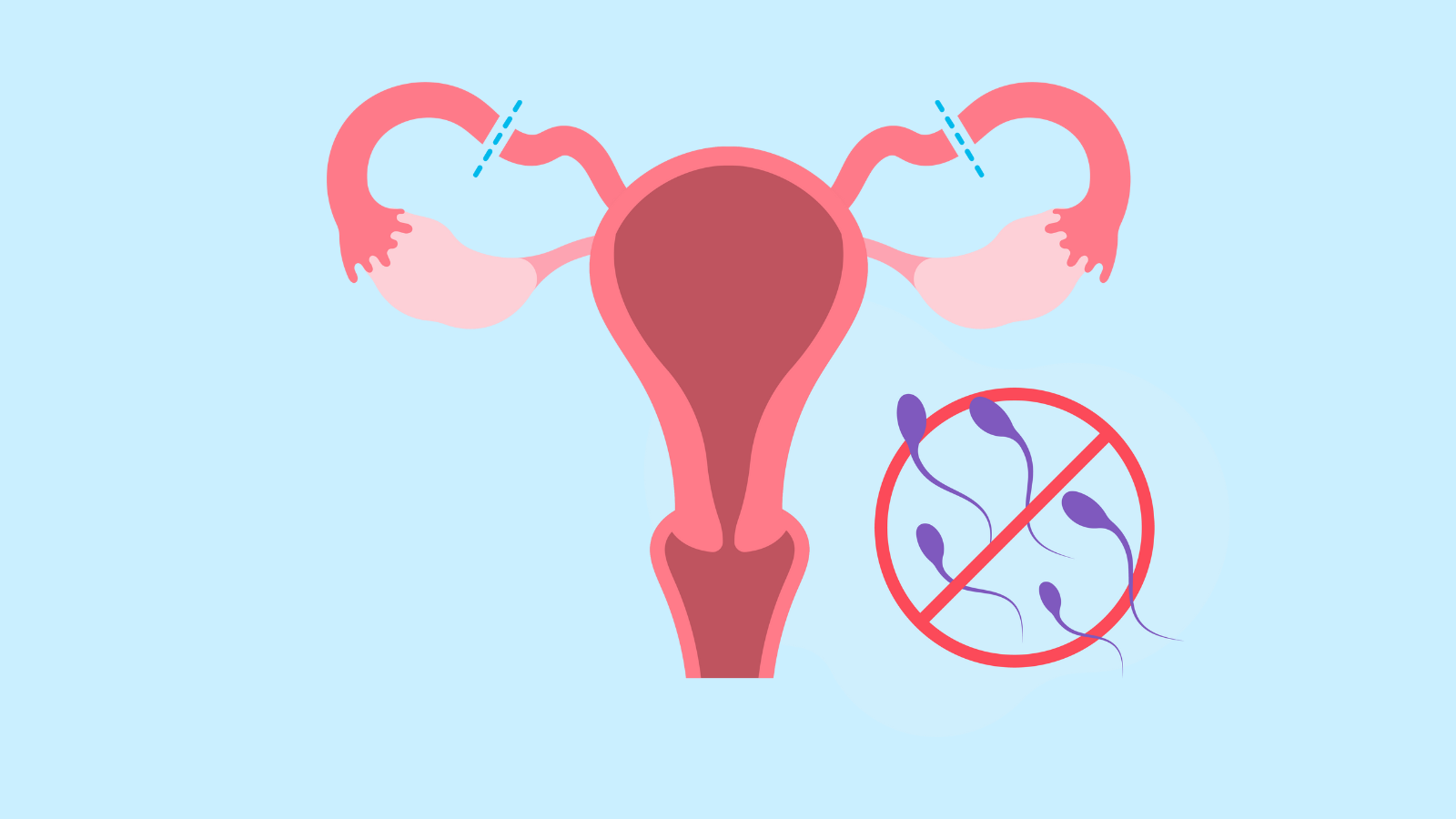


Many of the birth control methods on the market today rely on hormones to prevent pregnancy mostly by suppressing ovulation. Hormonal birth control methods are among the most effective, and hormones are safe for most people. But some people shouldn’t use hormones because of health conditions and other may prefer not to. There are some good non-hormonal options.
Non-hormonal contraceptive methods fall into a few categories. First, you can make sure that sperm and egg never meet by changing your behavior so that you’re practicing abstinence some or all of the time or pulling out before ejaculation. Behavioral methods can be effective as long as both partners are committed to following through all the time. However, there are many more effective methods available.
There are also some IUDs that do not contain hormones. They work by blocking the movement of sperm toward the egg.
You can also use a method that serves as barrier between partners like a condom, diaphragm, or cervical cap. These methods make sure that sperm and egg can’t meet. By covering the penis and preventing the exchange of bodily fluids, condoms also provide protection against sexually transmitted infections (STIs).
Finally, you can have surgery that blocks the vas deferens or the fallopian tubes so that sperm and eggs can’t get to their usual meeting places. This is called surgical sterilization, and it is permanent.
This page is going to focus on barrier methods and surgical sterilization. Check out other pages on the site for more information on other non-hormonal methods like the copper IUD, condoms, and behavior-based methods (like celibacy and fertility awareness).
In addition to condoms, there are three barrier methods on the market that you could choose from. The diaphragm, the cervical cap, and Phexxi which is an all-natural gel.
The spermicide has chemicals that stop sperm from moving. If sperm do make it around the barrier, the spermicide will make sure they don’t go any further.
Most diaphragms come in multiple size because people come in multiple size. You want the diaphragm to fit snuggly in you pelvis under your cervix with no room around it for sperm to get by. This means that you have to be fitted by a health care provider. The provider will give you a prescription for the correct size which you can fill at a pharmacy. A diaphragm can last for about two years, but if you gain or lose 10 or more pounds, or you have a baby, you need to be fitted again because your size may have changed.
Diaphragms should be covered by insurance. If you don’t have insurance, a diaphragm will cost somewhere between $85 and $250. The spermicide is available over the counter and costs around $10 or $15, but one kit (a tube of gel and an applicator) should last awhile.
You can put your diaphragm in before you have sex but if it’s been more than a few hours, you should add more spermicide inside the vagina. You should also add spermicide inside the vagina each time you have sex that day. Do not take out your diaphragm to do this, instead use an applicator like the one you might use with yeast infection medication.
You have to leave your diaphragm in for about 6 hours after sex to make sure that the spermicide has done its job. Keep in mind you can only leave the diaphragm in for 24 hours total, so you have to do some math to figure out when you to stop having sex.
When you’re ready to remove it, you can use your finger to grab the edge and pull it out. Wash it gently with soap and water and put it away for the next time.
Diaphragms are 94% effective if used correctly every time but only 83% effective in real life situations. That’s because there are a lot of steps to using a diaphragm, and people sometimes make mistakes. The most common mistake is not using it every time you have sex.
The small size is for people who have never been pregnant. The medium size is for people who have been pregnant but didn’t have a full-term vaginal birth because they had a miscarriage, an abortion, or delivered via C-section. The large size is for people who had one or more vaginal births.
You need a prescription for FemCap, but because the sizes are based on your history and not your body, telehealth works just as well as an in-person visit. Once you have the prescription, you can get the cervical cap through the company’s website. The cervical cap should be covered by insurance and available at no-cost to you. If you don’t have insurance, it will cost $110. Cervical caps have to be used with spermicide that usually cost about $10 to $15 dollars for a tube and an applicator.
To use a cervical cap, you put a dime-size dollop of spermicide on the inside, a little more on the outside, and spread some to cover the rim. Then you insert it, cup side in and push it all the way up, so that it’s covering your cervix. You can put it in ahead of time and leave it in for up to 48 hours. If you have penis-in-vagina sex more than once, you should add spermicide to the vagina with an applicator every time. Do not take the cap out to do this.
Wait 6 hours after the last time you had sex and then take the cap out by hooking your finger through the removal strap and pulling down. Wash it carefully and put it away for the next time.
If you’ve never had a full-term vaginal delivery, the cervical cap is about 86% effective under typical conditions. If you have had one or more full-term vaginal deliveries, the cervical cap is only about 71% effective. People who have had vaginal deliveries may want to choose a different method.
It is made from all natural ingredients including lactic acid, citric acid, and potassium bitartrate (also known as cream of tartar). Phexxi comes in pre-filled applicators that you insert into the vagina right before you have sex.
Phexxi works by keeping the pH in the vagina too acidic for sperm to survive. You have to put a new applicator of Phexxi into the vagina every time you have sex. If it’s been an hour or more since you inserted the gel and you haven’t had sex yet, you need to put a new applicatorful in before you do.
If you use Phexxi perfectly, it’s 93% effective. In real life situations, however, it’s been found to be about 86% effective.
Phexxi is only available with a prescription. If you have insurance, it may be free. For people without insurance, it costs $389 for a box of 12 pre-filled applicators. The manufacturer offers a discount program that may make it less expensive.
Barrier methods can be a good choice for people who shouldn’t or don’t want to use hormones, because you only have to think about them when you’re going to have sex.
They are not as effective as other methods and do require some effort. You have to be comfortable putting your fingers inside your body to insert and remove devices and/or using an applicator to put gel into your vagina. Some people find diaphragms and cervical caps difficult to insert and remove, but others have no issues with that. Because all of these methods require a gel of some kind, they can be messy. They can also cause vaginal irritation and more frequent UTIs. If you’re prone to UTIs, talk to your health care provider about whether these are the right methods for you.
Barrier methods other than condoms do not provide any protection against STIs.
People who are sure that they never want to be pregnant (again) or never want to get someone pregnant (again) should consider surgical sterilization. These are procedures that tie or remove the fallopian tubes or the vas deferens to prevent sperm and egg from meeting.
Remember, to get someone pregnant sperm have to leave the testicles, travel through the urethra, out the penis, and then travel through the cervix and uterus to the fallopian tubes where they may find an egg. Cutting or removing either the vas deferens or the fallopian tubes can prevent this.
Vasectomies should be covered by insurance but can cost as much as $2,000 without insurance.
Recovery can be uncomfortable. You may have to spend a couple of days sitting with ice packs on the area, but most men are fully recovered within a week to ten days. You should refrain from any sex or masturbation for the first week. Once you do start having sex again, continue to use another form of contraception until your three-month follow-up appointment. At this appointment, your provider will ask for a semen sample and test it to make sure there are no sperm.
If you get a vasectomy, your testicles will still make testosterone and produce sperm, but the sperm can’t go anywhere. They will simply die and be reabsorbed into your body. When you ejaculate your semen will be the same as it’s always been. The consistency, amount, appearance, and taste will not change. It’s only if you looked under a powerful microscope that you could tell that there aren’t any sperm in your ejaculate. Sexual performance, orgasm, and enjoyment also don’t change.
A vasectomy is almost 100% effective. You may have heard anecdotes of people who got someone pregnant after getting snipped, but this is very rare. Once your provider has checked that you’re not releasing sperm, you are essentially infertile. This procedure should be considered permanent.
While some people do have vasectomies reversed, that is a very complicated micro-surgery that often does not work. Only think about getting a vasectomy if you are sure that you do not want to get someone pregnant at any point in the future.
These are both surgical procedures that are typically done under general anesthesia (meaning you will be asleep during it). Sometimes these procedures are done when your abdomen is already open for another surgery or for a c-section delivery. Otherwise, they are usually done laparoscopically. This means that the surgeon doesn’t have to make a big incision, and you won’t have a big scar. It should also mean that recovery is easier. Most people recovery fully within a few days or a couple of weeks.
Having your fallopian tubes tied or removed does not affect your menstrual cycle, hormones, or sex life. You will ovulate as usual. Instead of traveling into the fallopian tube, the egg will go into your abdomen and will be reabsorbed by your body. Nothing else in your cycle should change.
Both procedures almost 100% effective. They are also both permanent. Some people who have had tubal ligations have had surgeries to try to recreate the fallopian tubes, but this is very complicated and there is no guarantee that it will be successful. Only consider surgical sterilization if you are sure you never want to get pregnant in the future.
Tubal ligation or salpingectomy should be covered by insurance. If you don’t have insurance, the procedures can cost as much as $6,000.
Surgical sterilization is permanent, almost 100% effective, and has no side effects after a brief recovery. Anyone who does not want to be pregnant or get someone pregnant in the future should consider sterilization.
If a heterosexual couple who plan to be together for a long time has decided they’re done having children and has started thinking about one partner getting sterilized, most providers would suggest that the man be the one to have the procedure. Vasectomies are simpler and less invasive, they do not require general anesthesia, and the recovery tends to be shorter and easier.

In the U.S., HPV infections are estimated to cause about 37,300 cases of cancer. The HPV vaccine can prevent over 90% of these cancers from ever developing.

Many methods of birth control that are available today rely on hormones like those that our bodies make naturally. Hormonal methods come in many different forms—from pills to patches to shots—but all of them essentially work the same way.

Anyone who is having penis-in-vagina sex runs the risk of getting pregnant every time they have sex. Even if it’s your first time. Even if you have your period. Even if it’s a full moon and Mercury is in retrograde.

A new study found that there are two distinct types of BV infection, one of which increases the risk of chlamydia infection.

Many STIs have no signs or symptoms in the majority of people infected. The only way to know if you have an STI is to get tested.
Sexually transmitted infections, or STIs—also called sexually transmitted diseases, or STDs—affect people of all ages, backgrounds, and from all walks of life. In the U.S. alone there are about 20 million new cases of STIs each year.

The condom. All sorts of shapes, sizes, colors (even glow-in-the-dark). Ribbed or plain. Lubed or not. Latex or plastic. ASHA’s Fred Wyand shares his thoughts on this reliable way to prevent STIs and pregnancy.
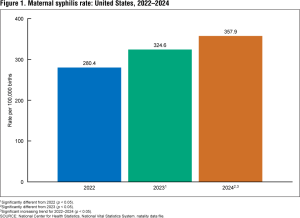
Syphilis rates among pregnant women went up 222% percent between 2016 and 2022 and another 28% between 2022 and 2024. This alarming increase shows too many pregnant women are not being screened.
Check out featured resources and the latest news on sexual and reproductive health.
The World Health Association recently declared a global health emergency amid rising cases of mpox. The current outbreak, which began in the Democratic Republic of Congo (DCR), is caused by a deadlier form of the virus than the one that spread throughout the world in
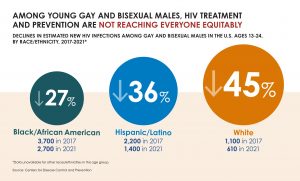
While CDC reported a decline in overall new HIV infections, disparities in HIV prevention and treatment remain.
ASHA believes that all people have the right to the information and services that will help them to have optimum sexual health. We envision a time when stigma is no longer associated with sexual health and our nation is united in its belief that sexuality is a normal, healthy, and positive aspect of human life.
ABOUT
GET INVOLVED
ASHA WEBSITES
GET HELP
© 2026 American Sexual Health Association
We need to know if we can keep you company during this visit. We are useful for making this site work.
We use cookies to enhance your browsing experience. You can choose which cookies you want to accept.
Necessary cookies help make a website usable by enabling basic functions like page navigation and access to secure areas. The website cannot function properly without these cookies.
| Cookie | Provider | Purpose | Expiry |
|---|---|---|---|
digiconsent | This website | Stores your cookie consent preferences. | 1 year |
wordpress_logged_in_* | WordPress | Identifies logged-in users and their authentication details. | 14 days / Session |
wordpress_sec_* | WordPress | Stores authentication details for secure areas. | 14 days / Session |
wp-settings-* | WordPress | Stores user interface customization preferences. | 1 year |
wp-settings-time-* | WordPress | Stores the time when wp-settings cookie was set. | 1 year |
Analytics cookies help us understand how visitors interact with our website by collecting and reporting information anonymously. This helps us improve our website.
Marketing cookies are used to track visitors across websites. The intention is to display ads that are relevant and engaging for the individual user.
Functional cookies enable the website to provide enhanced functionality and personalization. They may be set by us or by third party providers.