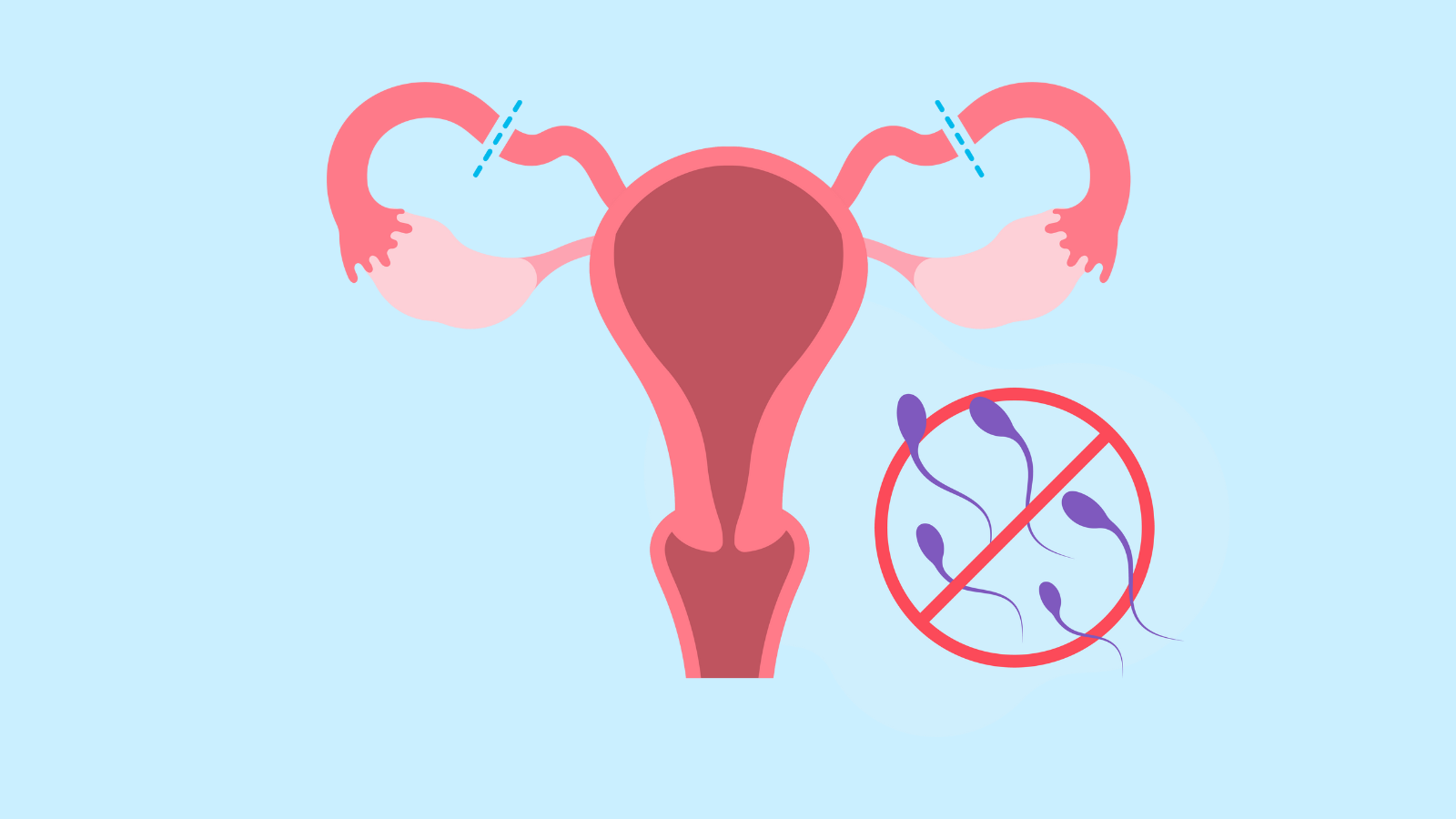
Contraception and Birth Control Methods
Anyone who is having penis-in-vagina sex runs the risk of getting pregnant every time they have sex. Even if it’s your first time. Even if you have your period. Even if it’s a full moon and Mercury is in retrograde.